We are going to cover Premature Fetus | Abruptio Placentae | Placenta Topic. In this post we firstly discuss basic Definitions and then FAQs.
Premature Fetus
A woman goes through a full-term pregnancy for roughly 40 weeks starting on the first day of her last period. The baby is regarded as full-term if it is born between weeks 38 or 39 to 42.
So, what is premature fetus? Medical professionals and organizations have slightly different definitions, but generally speaking, a fetus is considered premature and the birth is referred to as preterm when it occurs at 37 or 38 weeks or earlier and it is called as premature fetus.
The estimate is made using the mother’s last period date, measurements taken by ultrasound while the baby is still inside the uterus, and a direct examination following birth to determine the infant’s physical and neurological development.
Abruptio Placentae
One of the main reasons of vaginal bleeding in the second half of pregnancy is known as Abruptio Placentae, which is traditionally defined as the premature separation of the placenta before birth. One of the main factors contributing to maternal morbidity and perinatal mortality is abruptio placentae . Obstetric haemorrhage, the requirement for blood transfusions, an emergency hysterectomy, disseminated intravascular coagulopathy, and renal failure are among the dangers for mothers. Even though maternal deaths are uncommon, they occur seven times more frequently than average. Low birthweight, stillbirth, premature delivery, hypoxia, and neonatal death are all perinatal effects.
Abruptio
One of the most frequent causes of antepartum haemorrhage is abruptio, which is described as the early separation of a properly implanted placenta. In the second half of pregnancy, it is more prevalent. Abruptio placenta is a dangerous pregnancy condition that has a high death and morbidity rate for both mothers and newborns.
Placenta
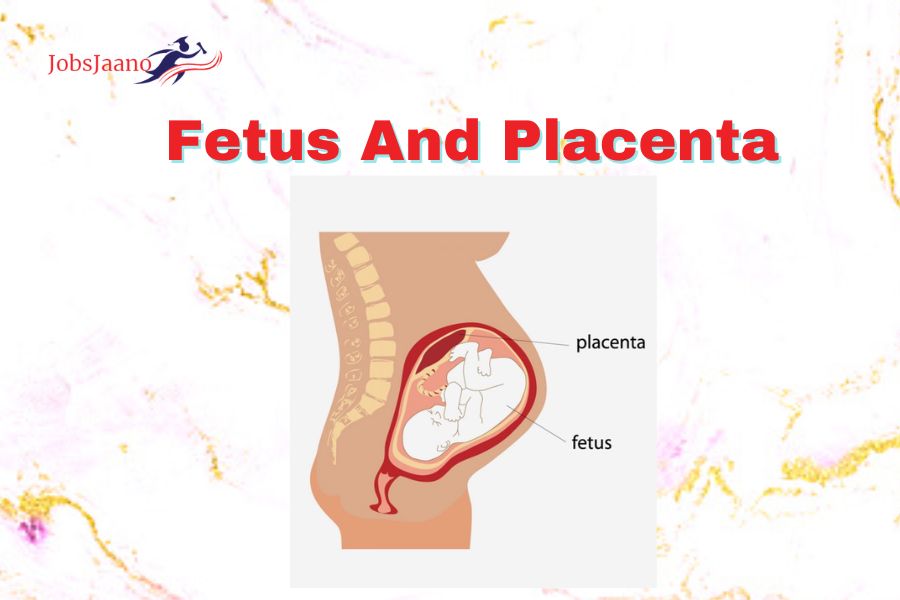
The human placenta is discoid because of its shape, haemochorial because of direct contact of the chorion with the maternal blood and deciduate because some maternal tissue is shed at parturition. The placenta is attached to the uterine wall and establishes connection between the mother and fetus through umblical cord.
It originates from the trophoblastic layer of fertilized ovum. It links closely with the mother’s circulation to carry out functions that the fetus is unable to perform for itself during intrauterine life. The survival of the fetus depends upon the placental integrity and efficiency.
Placenta is developed from two sources:
(a) Fetal Component: Which develops from the chorion frondosum.
(b) Maternal Component: It consists of decidua basalis.
The placenta is almost a circular disc, spongy fleshy structure, thick at centre but thin in edge.
Diameter: 15-20 cm
Thickness: 2.5 cm at its centre
Weight: 500 gms
Surface area: 243 sq. cm
Growth Restricted Fetus | Restricted fetal growth
A condition known as Restricted Fetal Growth (FGR) occurs when a foetus is smaller than anticipated for the number of weeks of pregnancy (gestational age). A common definition of it is a projected weight below the 10th percentile.
At any point during pregnancy, FGR can start. The baby’s growth is poor when FGR is present. FGR may have an impact on the baby’s total size as well as the development of its tissues, organs, and cells. Many issues may result from this. However, a lot of petite infants might just be that. They might not have any issues.
Decreased Fetal movement but strong heartbeat
Posterior placenta previa | real life placenta | detached placenta
Placenta previa is when the placenta attaches to the uterine wall where it partially or completely covers the uterine exit (opening of the cervix).
The most prominent sign of placenta previa is bleeding after the 20th week of pregnancy. A placenta previa diagnosis is made with an ultrasound examination.
Anterior placenta | posterior placenta | anterior low lying placenta | freezing placenta
If you have an anterior placenta, it will be found near the front of your uterus, nearest to your stomach. It is typical with pregnancy and is not a warning sign. At about 18 to 21 weeks of pregnancy, an ultrasound is used to make the diagnosis.
The placenta is joined to the uterus’s posterior wall. As “fundal” refers to the top of the fundus/uterus, the phrase “posterior placenta” denotes that the placenta is located nearer the top and back of the uterine wall.
Anencephalic fetus | normal heartbeat for fetus | male fetus ultrasound | dead fetus
Placenta real | preeclampsia placenta | placenta accreta spectrum | placenta blocking cervix
Accreta | partial placenta previa | ruptured placenta | keeping your placenta after birth
placenta covering cervix | placenta and cord | saving placenta after birth
Placenta accreta ultrasound | 27 week old fetus | keeping placenta
Irregular fetal heartbeat third trimester | 5 month fetus | accreta pregnancy
FAQs
Q.1. From where does placenta develop?
Ans. It develops from fetal chorionic tissue and maternal decidua during pregnancy.
Q.2. Where does it get implanted?
Ans. It is implanted on the uterine wall.
Q.3. With which structure is it connected to the fetus?
Ans. It is connected with fetus through umbilical cord in the amniotic cavity.
Q.4. What is the purpose of placenta?
Ans. It maintains pregnancy and carries vital fetal functions.
Q.5. At which week is placental site located by ultra sound?
Ans. By 8th week, placental site can be located by ultrasound.
Q.6. Name the types of Placental Villi.
Ans. There are 2 types of placental villi:
(a) Anchoring Villi.
(b) Nutritive Villi.
Q.7. Give an example of acceptance of Immunological Acceptance of the fetal graft by the mother.
Ans. The fact that maternal and fetal tissue come in direct contact without rejection suggests immunological acceptance of the fetal graft by the mother.
Q.8. When is the interstitial implantation completed?
Ans. Interstitial implantation is completed on 11th day.
Q.9. When do the Stem Villi develop?
Ans. Stem villi develop on the 13th day.
Q.10. What is the purpose of the Stem Villi?
Ans. It connects the chorionic plate with the basal plate.
Q.11. From where do the Primary, Secondary Tertiary Villi develop?
Ans. These develop from Stem Villi.
Q.12. What is the system called which make connection with the intraembryonic vascula system?
Ans. It is called Arterio-Capillary-Venous System.
Q.13. Through what is Intraembryonic vacula system connected with Aeterio-capillary-venou system.
Ans. Body Stalk.
Q.14. At last which 2 parts form the discret Placenta?
Ans. These two, chorion frondosum and decidua basalis form the discrete placenta. get
Q.15. When does placenta formation start and completed?
Ans. It begins at 6th week and is completed by 12th week.
Q.16. What is the shape of placenta at term?
Ans. It is circular disc.
Q.17. What is diameter and thickness?
Ans. Diameter →15-20 cm
Thickness at its centre →2.5 cm
Q.18. Write the weight of placenta at term?
Ans. It is about 500 gms in weight.
Q.19. How much part of Uterine Wall does occupy?
Ans. It occupies 30% of Uterine Wall.
Q.20. How many Surfaces does it have?
Ans. It presents two surfaces.
(a) Fetal and Maternal. (b) Peripheral Margin.
Q.21. At term how much part of placenta is of Fetal Origin?
Ans. At term about 4/5th of placenta is of Fetal Origin.
Q.22. How Many lobes/Cotyledons does the Maternal surface of placenta consist?
Ans. It consists of 15-20 lobes, which are limited by fissures.
Q.23. How much part of placenta is of Maternal origin?
Ans: 1/5th part
Q.24. Of which layer is placenta a specialised part?
Ans. Chorion placenta is a specialised part of chorion.
Q.25. Name the line of separation of placenta after birth of baby.
Ans. Decidua spongiosum.
Q.26. By which structures is placenta limited
Ans. Placenta is limited internally (fetal aspect) by the internally?
(a) Amniotic Membrane &
(b) Chorionic Plate.
Q.27. By which structures is placenta limited externally?
Ans. Placenta is limited externally (maternal aspect) by the basal plate.
Q.28. What all lies in between the external basal plate and internal choronic plate?
Ans. Between these 2 lies the intervillous space containing the stem villi with their branches, the space being filled with maternal blood.
Q.29. List the types of Circulation in Placenta.
Ans. Placental circulation consists of independent circulation of blood in 2 systems. (i) Uteroplacental Circulation. (Maternal Circulation)
(ii) Feto-Placenta Circulation.
Q.30.Define Maternal Circulation or Uteroplacental Circulation.
Ans. It is concerned with the circulation of the maternal blood through the intervillous space.
Q.31. How much volume of blood does a Mature Placenta have?
Ans. A mature placenta has a volume of about 500ml of blood. In this, 350ml is occupied in the villi system and 150ml lies in the Intervillous space.
Q.32. From where do the villi get nutrition?
Ans. It gets nutrition from the maternal blood.
Q.33. Write the pressure within intervillous space during uterine relaxation and uterine contraction.
Ans. Pressure during Uterine Relaxation = 10-15 mmHg. Pressure during Uterine Contraction= 30-50 mmHg.
Q.34. How much is the fetal capillary pressure in the villi?
Ans. It is 20-40mmHg.
Q.35. Which blood vessels carry the arterial circulation?
Ans. Spiral arteries.
Q.36. How is the Venous drainage carried?
Ans. By Uterine Veins.
Q.37. In Feto-Placental Circulation what do the Umbilical arteries carry?
Ans. The 2 Umbilical arteries carry Impure blood from the fetus.
Q.38. How much is the fetal blood flow per minute through placenta?
Ans. It is about 400ml per minute.
Q.39. What is the pressure in Umbilical artery?
Ans. It is 60mmHg.
Q.40. What is the pressure in Umbilical vein?
Ans. It is 10mmHg.
Q.41. Define placental Barrier or Placental Membrane.
Ans. Placental barrier is a barrier which separates the maternal and fetal blood.
Q.42. What is the purpose of Placental barrier?
Ans. Its purpose is that, in spite of close proximity there is no mixing of maternal and fetal blood.
Q.43. List the layers of the placental membrane.
Ans. It consists of:
(a) Syocytiotrophoblast.
(b) Cytotrophoblast.
(e) Endothelium of the fetal capillary wall with its basement membrane.
(c) Basement membrane.
(d) Stromal Tissue.
Q.44. What is the thickness
Ans. It is about 0.025mm thick.
Q.45. Define Placental Ageing.
Ans. Placental ageing is the ageing process that involves both the fetal and maternal components. As the placenta has got a limited lifespan it is likely to undergo degenerative changes as a mark of senescence (Pertaining to old age). During placental ageing changes occur in
(a) Villi
(b) Decidua &
(c) Intervillous space.
Q.46. Enumerate the Placental functions. Ans. Placenta has the following functions:
(a) Respiratory functions.
(b) Excretory functions..
(c) Nutritive functions.
(d) Transfer functions.
(e) Enzymatic functions.
(f) Barrier functions.
(g) Immunological functions.
Q.47. Name the fetal membranes.
Ans. The fetal membrane consists of 2 layers.
1. The Outer – Chorion.
2. The Inner Amnion.
Q.48. Does chorion have Vessels or Nerves?
Ans. Not at all, it has no vessels or nerves,
Q.49. Can amnion be peeled off?
Ans. Yes, it can be peeled off from the fetal surface of the placenta except at the insertion of umbilical cord.
Q.50. Define Amniotic Cavity.
Ans. The fluid filled space which appears between the ectodermal layer and the cytotrophoblast is called amniotic cavity.
Q.51. Where & how does liquor amnii surround the fetus?
Ans. Liquor amnii surrounds the fetus everywhere except at its attachment with the body stalk.
Q.52. What all is not present in amnion?
Ans. Amnion has got neither any lymphatic system.
Q.53. How much fluid does fetus drink at terma how much does the fetus excrete?
Ans. The fetus drinks about 400ml of liquor every & at term & equal amount is excreted in the Urine,
Q.54. Within how many hours does the
Ans. The water in the amniotic fluid is complete
Q.55. How much is the volume of amniotic fluid from 12 weeks till term?
Ans. It is as follows: 12 Weeks-50 ml
20 Weeks-400ml
36-38 Weeks- 1000 ml (1litre)
Hence at term it is 600-800ml.
Q.56. What happens to fluid in post-term pregnancy?
Ans. As the pregnancy continues post term, further Ans reduction occurs to the extent of about 200ml at 43 weeks.
Q.57. Write the physical features of Amniotic Fluid.
Ans. (a) The fluid is faint alkaline.
(b) Its specific gravity is 1.010.
(c) At term pregnancy it becomes highly hypotontic to maternal serum.
Q.58. What range of Osmolarity is indicative of fetal maturity?
Ans. An Osmolarity of 250m Osmol/ Litre.
Q. 60. Why does the Amniotic fluid become pale straw coloured and turbid at term?
Ans. It may look turbid-due to presence of vernis caseosa & pale straw coloured due to the presence of exfoliated lanugo & epidermal cells from the fetal skin.
Q.62. Define Funis.
Ans. It is also called as Umbilical cord. It forms the connecting link between the fetus and placenta through which the fetal blood flows to and from the placenta. It reaches the placenta’s foetal surface from the foetal umbilicus.
Q.63. From where is this funis developed?
Ans. The Umbilical cord is developed from the body stalk or connective stalk which is a band of mesoblastic tissue. stretching between embryonic disc and chorion.
Q.64. List the structures that cover the funis.
Ans.
- Covering epithelium.
- Wharton’s jelly (has protective functions)
- Blood vessels (2 arteries & 2 veins-4 vessels)
- Remnant of the Umbilical Vesicle (Yolk sac) &
- Obliterated extra embryonic coelom.
Q.65. What is eccentric insertion?
Ans. When the placenta attaches to the fetal surface of placenta, somewhere between the centre and the edge of placenta, it is called as eccentric insertion.
Q.66. Define Velamentous insertion?
Ans. When the attachment is central, marginal or even on the chorionic laeve at varying distance, away from the margin of the placenta, it is called velamentous insertion.
Q.67. In the early periods where is the cord attached?
Ans. In early periods, cord is attached to the ventral surface of embryo close to the caudal extremity.
Q.68. Where does the cord attachment shift at 4th month and why?
Ans. At 4th month it is moved permanently to the centre of abdomen, as the coetom closes and yolk sac atrophies.
Q.69. What is the normal length of the cord?
Ans. It is 50 cm or ranges from 30-100 cm.
Q: 70. What is its diameter?
Ans. Average 1.5cm with variation of 1-2.5 cm.