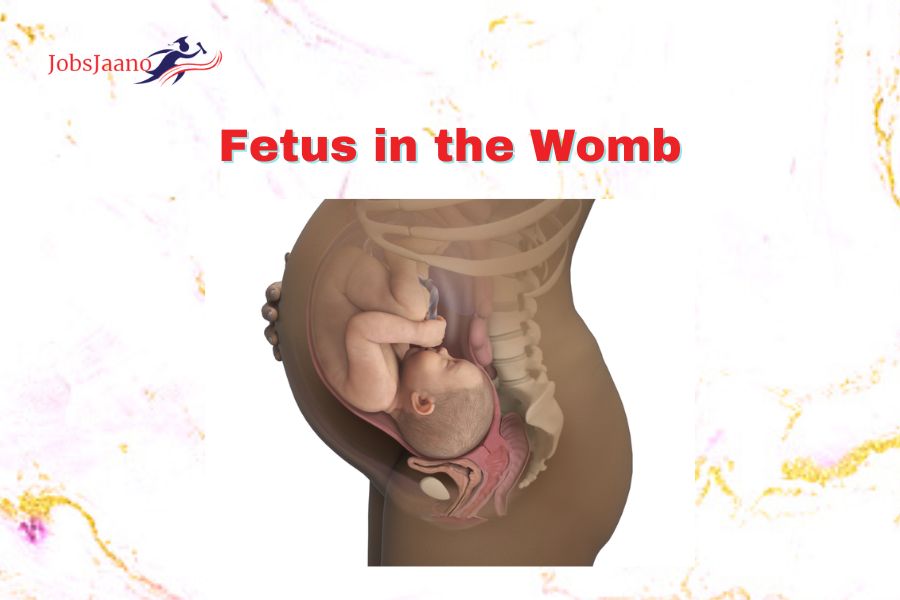
Let us discuss the detail knowledge of fetus in the womb.
- LIE
(a) The lie refers to the relationship of the long axis of the centralised uterus or maternal spine.
(b) The commonest being – Longitudinal (99.5%)
(c) The lie may be transverse or oblique or sometimes unstable until labour sets in and after this it becomes longitudinal or transverse.
- PRESENTATION
The part of fetus which occupies the lower pole of uterus is called presentation of the fetus.
The presentation may be :
(a) Cephalic (96.5%)
(b) Podalic (3%)
(c) Shoulder and other (0.5%)
Note: When more than one part of the fetus is present it is called compound presentation.
- PRESENTING PART
The presenting part is defined as the part of the presentation which lies over the internal orifice (Os) and is felt by the examining finger through the cervical opening. Thus in
(a) Cephalic presentation-Presenting part is vertex (96%) (Commonest)
(b) Brow or face depending upon the degree of flexion of head (0.5%)
(c) The presentation may be
(i) Complete breech – Fetal legs flexed
(ii) Frank breech – Fetal legs extended.
(iii) Footling presentation-Foot may be present.
- ATTITUDE
The term “attitude” refers to how the various components of the foetus relate to one another. The universal attitude is of flexion but there may be exceptions to this universal attitude and extension of head may occur (deflexed vertex, brow or face presentation according to degree of extension.)
- DENOMINATOR
It is the relation of the denominator to the different quadrants of pelvis. Theoretically there are 8 positions divided into equal segments of 45 degree to place the denominator in each segment.
(a) L.O.A (Left Occipito Anterior) Commonest and called the first vetex position.
(b) R.O.A (Right Occipito Posterior) 2nd Vertex Position
(c) R.O.P (Right Occipito Posterior) 3rd Vertex Position
(d) R.O.T (Right Occipito Transverse)
OBSTETRICAL EXAMINATION | Obstetrics Initial Exam | Annual Gynecologic Exam
The methods of Obstetrical examination are as follows:
- Abdominal Examination.
- Internal Examination.
- Sonar or Radiology.
-
ABDOMINAL EXAMINATION Abdominal Examination includes:
(a) Inspection
(b) Palpation. It includes Obstetric grips
(i) Fundal grip
(ii) Lateral or Umbilical grip
(iii) First pelvic grip
(iv) Second pelvic grip (Pawlik’s grip).
(c) Ascultation.
(a) Inspection
Inspection is done to note:
(i) Whether the Uterine Ovoid is longitudinal or transverse or oblique.
(ii) Contour of uterus-i.e. Convex or flattened anterior wall, fundal notching, spherical or cylindrical shape
(iii) Undue enlargement of uterus.
(iv) Skin condition of abdomen to note ringworm or scabies.
(v) Further inspection is done to note any incisional mark on the abdomen.
(b) Palpation
It is done to note the height of uterus. The palpation should be done gently. One should keep in mind that during braxton hicks contraction or uterine contraction in labour palpation should be suspended. Palpation includes Obstetric grips and these are as follows:
(i) Fundal Grip
The palpation in Fundal grip is done facing the patients’s face.
The whole fundal area is palpated using both hands laid flat on it to find which pole of fetus is lying in the fundus:
Broad, soft irregular mass is suggestive of breech.
Smooth, Hard & Globular mass is suggestive of head.
Both foetal poles cannot be felt in the fundal region of a woman in transverse lie.
(ii) Lateral/Umbilical Grip
The palpation is done facing patient’s face.
Both the hands are placed flat on either side of the Umbilicus to palpate one after another.
By palpation one notes the position of back, limbs and anterior shoulder.
The smooth, curved, and unyielding feel alludes to the back.
The limb side is empty and there are small knob like irregular parts.
After above 2 the position of Anterior shoulder is found. It is present as a prominence in the lower part of uterus above the head.
(iii) First Pelvic Grip
The examination is done facing the ‘Patient’s feet’.
In the lower pole of the uterus, four fingers from each hand are positioned on either side of the midline.
The fingers are pressed downwards and backward to palpate the part occupying the lower pole of uterus.
It is head, the characterstics to note are:-
Precise presenting part.
Attitude
Engagement
- iv) Second Pelvic Grip Or Pawlik Grip
(i) The examination is done facing towards the patient’s face. the
(ii) The over stretched thumb and 4 fingers of the right hand are placed over the lower pole of uterus (keeping the ulnar border of the palm on the upper border of symphysis pubis)
(iii) When the fingers & thumb are approximated the presenting part is grasped distinctly, if not engaged, and also the mobility from side to side is tested. In transverse lie Pawlik grip is absent.
(c) Auscultation
Auscultation of fetal heart sounds helps to diagnose a live baby only.
It is heard at different parts according to the presentation of the uterus. For example:
(i) In Vertex & breech presentation: The fetal heart sounds are best audible through the back.
(ii) In face presentation: It is heard through fetal chest.
As a rule maximum intensity of the F.H.S. is below the umbilicus in cephalic & around the umbilicus is Breech. In Occipito lateral it is heard laterally & in Occipito posterior it is heard towards the flanks-In left occipito posterior it is difficult to locate the F.H.S.
- INTERNAL EXAMINATION:
It helps in diagnosis of presentation and position through the vaginal examination.
- SONAR OR RADIOLOGY:
X-rays help to diagnose pregnancy. Ultrasonography can locate the head & body of fetus.
FETAL SKULL
The foetal skull is mostly made up of thin, malleable tabular (flat) bones that constitute the vault and is somewhat compressible. The inflexible and rigid bones at the skull’s base serve as a foundation for this.
(A) AREAS OF SKULL
The skull is divided into several zones of Obstetrical importance. These are
(i) Vertex
(ii) Brow
(iii) Face.
(i) Vertex
It is a quadrangular area bounded anteriorly by bregma and coronal sutures posteriorly/ behind by the lambda and lambdoid sutures.
By lines that cut through the parietal eminences on the side.
(ii) Brow
It is an area bounded on one side by the anterior fontanelle and coronal sutures and on the other side by root of the nose and supra-orbital ridges of either side.
(iii) Face
It is an area bounded on one side by the root of the nose and supra-orbital ridges and on the other, by the junction of the floor of the mouth with neck.
SUTURES AND FONTANELLE
Non-ossified membranes linked to the bone borders hold the flat bones of the vault together. These are called sutures and fontanella.
SUTURES
There are mainly 4 types of sutures.
(a) The saggital or longitudinal suture: It lies between two parietal bones.
(b) The Coronal Suture: Located on either side of the parietal and frontal bones.
(c) The Frontal Suture: It lies between two frontal bones.
(d) The Lambdoid Suture: It separates the Occipital bone and the two parietal bones.
FONTANELLES
A wide gap in the suture line is called Fontanella.
TYPES
Of Many fontanella (6 in number) only 2, are of Obstetric significance. These are
- Anterior fontanelle (Bregma)
- Posterior fontanelle (Lambda)
-
Anterior Fontanella (Bregma):
(a) It is formed by joining of the 4 sutures in the midplane. These are:
(i) Anteriorly: Frontal Suture
(ii) Posteriorly: Saggital Suture
(iii) Laterally or either side: Coronal Suture
(b) Shape of Anterior Fontanella: Diamond Shaped.
(c) Measurements of Anterior Fontanella
(i) Anteroposterior diameter: 4 cm
(ii) Transverse diameter: 2.5 cm.
(d) Time of Ossification of Anterior Fontanelle: It is 18 months after birth.
Posterior Frontanelle (Lambda)
(a) It is formed by the junction of 3 suture lines anteriorly: Sagittal suture.
(b) Laterally or either side: Lambdoid suture.
(c) Shape of Posterior Frontanelle: Triangular shaped
(d) it measures about 1.2 cm
(e) time of ossification: 6-8 weeks
TRANSVERSE DIAMETERS
- Biparietal diameter-(9.5 cm) It extends between two parietal eminences. No matter where the head is positioned, this diameter almost always engages.
- Super: From a point above the other parietal eminence on the opposite side, there is an 8.5 cm subparietal distance.
- Bi: Temporal diameter; (8 cm) It is the distance between the anterior-inferior ends of the coronal suture.
- Bi: Mastoid diameter: 7.5 cm: It is the distance between the tips of the mastoid processes.
BONY PELVIC
- The Bony Pelvic or Articulate Pelvic is Composed of 4 Bones
(a) 2 innominate bones
(b) Sacrum (1)
(c) Coccyx (1)
- Joints of Pelvis
The above 4 units together to form 4 joints
(a) 2 Sacroilliac Joints
(b) 1 Sacrococcygeal joint
(c) Symphysis pubis.
- ANATOMICAL DIVISIONS OF BONY PELVICS
The bony pelvis is anatomically divided into:
(a) False Pelvis
(b) True Pelvis, it is divided into – 3 Parts:
(i) Inlet
(ii) Cavity &
(iii) Outlet.
(a) The False Pelvis
It is formed by the illiac portions of the innominate; bones and is limited above by the illiac crests.
It has got little Obstetric significance that is to support the enlarged uterus during pregnancy.
Boundaries of false Pelvis
(i) Posteriorly: Lumbar Vertebrae
(ii) Laterally: Illiac fossa.
(iii) Anteriorly: Anterior abdominal wall.
(b) The True Pelvis
The true pelvis forms the canal through which the fetus has to pass. It is 4 cm deep and shallow in the front due to the symphysis pubis. measures 11.5 cm and is posteriorly created by the sacrum and coccyx. It is divided into:
(i) Inlet
(ii) Cavity &
(iii) Outlet.
(i) The Inlet
Inlet is the Brim of the pelvis. The previously stated bone features define the inlet’s perimeter.
Dimeters of Inlet
Antero-posterior diameter
- Oblique diameter
- Transverse diameter.
Conjugates
- Obstetric Conjugate
- Diagonal Conjugate
Diameters
Antero-posterior diameter
or True conjugate or = 11 cm.
Anatomical Conjugate or Conjugate Vera. it is the distance between the midpoint of sacral promontory to the inner margin of upper border of symphysis pubis. It measures 11cm.
Oblique Diameter: 12 cm.
There are 2 oblique dimeters: right and left
From one sacroiliac joint to the opposing illiopubic eminence, each one extends.
The sacro-illiac joint from which it originates is indicated by right or left.
Transverse Diameter: 13 cm.
It is the distance between the two farthest point on the pelvic brim over the iliopectineal lines. It measures 13 cm.
Conjugates
Obstetric Conjugate: It is the distance between the midpoint of sacral promontory to prominent bony projection in the mildine on the inner surface of the symphysis pubis. It measures in cm. It can be directly measured from subtracting 1.5-2cm from diagonal conjugate.
Diagonal Conjugate: It is the distance from the midpoint of the sacral promontory to the lower border of the symphysis pubis. It measures 12 cm.
-
Cavity
Cavity is the segment of the pelvis founded above by the inlet and below by plane of least pelvic dimensions. The cavity is round.
Diameters
Antero-posterior: 12 cm.
It measures the distance between the junction of the second and third sacral vertebrae and the midpoint on the posterior surface of the symphysis pubis.
Transverse: 12 cm.
Since the points are over the soft tissues that cover the sacrosciatic notches and obturator foramina, a precise measurement is impossible.
Outlet
The diameters of outlet are divided into 2. Obstetrical Outlet
Anatomical Outlet.
Obstetrical Outlet:
Transverse: 10.5 cm. It represents the separation of the tips of two ischial spines.
Antero-posterior: 11Cm. It extends from the inferior border of symphysis pubis to the tip of the sacrum.
Anatomical Outlet: It is known as the bony outlet and it is very important-There are 2 diameters:
Antero-posterior diameter– 13 cm. It extends from the lower border of symphysis pubis to the соссух.
Transverse diameter or Inter tuberous- 11 cm. It measures between inner border of ischial tuberosities.
Bony landmarks on the pelvis’ brim
From Anterior to posterior on each side:
Upper border of symphysis pubis.
Pubic Crest
Pubic Tubercle.
Pectineal Line.
Illiopubic eminence.
Illiopectineal line.
Sacroilliac articulation.
Anterior border of a/a of sacrum.
Sacral promontory.
FAQs
Q.1. Why is periodic examination important in the pregnancy?
Ans. Periodic examination is essential to note the:
(a) Lie.
(b) Presentation.
(c) Position.
(d) Attitude.
Q.2. What is Lie?
Ans. Lie refers to the relationship of the long axis of the fetus to the long axis of centralized uterus or maternal spine.
Q.3. What are the different Lie’s? Name the commonest of all.
Ans. The different Lie’s are as follows:
(a) Longitudinal.
(b) Transverse.
(c) Oblique.
(d) Unstable.
But the Commonest Lie is Longitudinal i.e. (99.5%)
Q.4. Define Presentation.
Ans. The part of the fetus which occupies the lower pole of uterus is called presentation of the fetus.
Q.5. Write the main presentations?
Ans. These are:
(a) Cephalic (96.5%)
(b) Podalic (3%)
(c) Shoulder and other (0.5%)
Q.6. Define Compound presentation.
Ans. When more than one part of the fetus present is called compound presentation.
Q.7. Describe the presenting part.
Ans. The presenting part is the part of presentation which overlies the internal Os.
Q.8. How is the presenting part felt?
Ans. The presenting part is felt with the examin finger through the cervical opening.
Q.9. Which the most commonest presenting part?
Ans. Vertex (Commonest).
Q.10. Define Attitude.
Ans. It is the relation of the different parts of the fe to one another.
Q.11. What is the Universal attitude of the fetus.
Ans. The Universal attitude of fetus is that of flexion.
Q.12. What do you understand by Denominator?
Ans. It is an arbitrary bony fixed point on the part which comes in relation with the various quadran of the maternal pelvis.
Q.13. Write the various denominators of different presentations.
Ans. The various denominators of different presentations are:
Occiput in vertex.
Mentum in face.
Frontal eminence in Brow
Sacrum in breech.
Acromion in shoulder.
Q.14. What is position?
Ans. It is the relation of the denomination to the different quadrants of the pelvis.
Q.15. Name the first four vertex position.
Ans. Name the first four vertex position are:
- L.O.A (Left Occipito Anterior) (First Vertex position)
- R.O.A (Right Occipito Anterior) (Second Vertex position)
- R.O.P (Right Occipito Posterior) (Third Vertex position)
- L.O.P (Left Occiptio Posterior) (Fourth Vertex position)
- The Commonest Position is L.O.A.
Q.16.What all is done before Abdominal Examination?
Ans. The preliminaries of abdominal examination are as follows:
(a) Ask the patient to evacuate or empty the bladder.
(b) Give her dorsal position with thighs slightly flexed.
(c) Expose the abdomen.
(d) Stand on the right side of patient and examine her.
Q.17. Why is Inspection done?
Ans. It is done to note:
(a) Whether the uterine Ovoid is longitudinal or transverse or oblique.
(b) Contour of Uterus.
(c) Undue enlargement.
(d) Skin condition of abdomen.
(e) Any incisional Scar Mark.
Q.18. Name of the Conditions where height of uterus is more than period of Amenorrhea.
Ans. Following are name of the Conditions where height of uterus is more than period of Amenorrhea:
(a) Mistaken date of last menstrual period.
(b) Twins pregnancy.
(c) Polyhydramnious
(d) Big baby
(e) Pelvic tumors
Ovarian
Fibroid
(f) Hydatidiform Mole
(g) Concealed accidental haemorrhage.
Q.19. List the conditions where height of uterus is less than period of Amenorrhea?
Ans. (a) Mistaken date of last menstrual period.
(b) Scanty liquor amnii.
(c) Fetal growth retardation.
(d) LU.F.D. (Intra Uterine fetal death).
Q.20. When should palpations be suspended?
Ans. During Braxton Hicks Contractions.
Q.22. In vertex & breech where are F.H.S. best Audible?
Ans. They are audible through the back.
Q.23. What does fundal grip find out?
Ans. It tells about the pole of fetus lying in fundus e.g.
(a) Broad, soft, irregular mass indicates breech.
(b) Smooth hard and alobular mass indicates head.
(c) In transverse lie neither of fetal poles are palpated in fundal area.
Q.24. What is found by lateral or Umbilical Grip?
Ans. It helps to find out the position of the back, Limbs and Anterior Shoulder e.g. the back is curved smooth & resistant. The limb side in empty.
Q.25. What does first pelvic grip indicate?
Ans. It helps to palpate the part occupying the lower pole of the uterus. (Presentation).
Q.26. Where is the maximum intensity of F.H.S. heard in cephalic presentation & breech?
Ans. In cephalic presentation F.H.S. is heard below Umbilicus.
Q.27. In which position the F.H.S is difficult to locate?
Ans. In Occipito-posterior position.
Q.28. What does ultrasonography locate?
Ans. It locates the Head & Body of the fetus.
Q.29. In Vertex Presentation write the following:
Ans. (a) Lie- Longitudinal
(b) Presentation -Cephalic
(c) Attitude-Flexed
(d) Denominator- Occiput
(e) Presenting Part-Vertex
(f) Position- Right Occipito Anterior
Or
Left Occipito Anterior.
Q.30. Define Engagement?
Ans. When the greatest horizontal plane, the biparietal, has passed the plane of pelvic brim, the head is said to be Engaged.
Q.31. What is the distance between the pelvic inlet and ischial spines?
Ans. It is about 5 cm.
Q.32. What can we infer if the head does not engage after 38th week in Primigravida?
Ans. If the head does not engage even after 38 weeks the following causes are to be sought out for
(a) Deflexed head placing the larger diameter to engage.
(b) Cephalo pelvic pelvic dispropertion
(c) Polyhydramnios.
(d) Poor formation of Lower Uterine segment,
(e) Hydrocephalous.
(f) Placenta praevia.
(g) Pelvic Tumours.
(h) High Pelvic Inclination.
(i) Functional- Where no cause can be detected
Q.33. Of What kind is the fetal skull and which type of bones is it made up of?
Ans. Fetal skull is to some exient compressible and made mainly of thin pliable tabular (Fiat) bones.
Q.34. What do these flat tabular bones form?
Ans. They form the vault.
Q.35. What are the Areas of Skull?
Ans. The areas of skull are:
(a) Vertex
(b) Brow
(c) Face.
Q.36. List the Sutures.
Ans. These are:
(a) The Saggital or Longitudinal Suture
(b) The Coronal Suture
(c) The frontal Suture
(d) The lambdoid Suture
Q.37. What is the importance of these Sutures?
Ans. Importance of these sututes are:
(a) It permits gliding movement of one bone the other during Moulding of head.
(b) Digital palpation of saggital Suture during internal examination in labour gives an idea the manner of engagement of head, degre internal rotation & degree of moulding head.
Q.38. Define fontanelle. Name the main Ones?
Ans. It is the Wide Gap in suture line. The main are:
(a) Anterior Fontanelle (Bregma).
(b) Posterior Fontanelle (Lambda).
Q.39. From how many sutures in is Anterior ontanelle made? name them.
Ans. It in formed by joining of the 4 sutures in the Midplane. The Sutures are:
Anteriorly- Frontal
Posteriorly- Sagittal
Laterally /on either side- Coronal
Q.40. What is the Shape of Anterior Fontanelle?
Ans. It is diamond shaped.
Q.41. When does the anterior fontanelle get Ossified & what happens if it does not?
Ans. It gets Ossified 18 months after birth. It becomes athological if it fails to ossify even after 24 months.
Q.42. What is the Importance of anterior fontanelle?
Ans. Anterior fontanelle is important for the following reasons:
(a) Through internal examination its palpation denotes the degree of flexion of head.
(b) It facilitates moulding of the head.
(c) Palpation of the floor reflects Intracranial status depressed in dehydration, elevated in ralsed intracranial status.
(d) Rarely cerebro spinal fluid can be drawn through the lateral angle of the anterior fontanella from the lateral ventricle.
(e) Rarely collection of blood and exchange transfusion can be performed through it via the superior longitudinal sinus.
Q.43. How is posterior fontanelle formed?
Ans. Posterior fontanelle is formed by junction of 3 suture lines:
Anteriorly- Sagittal suture.
Laterally/on either side- Lambdoid suture.
Q.44. What is the shape of posterior fontanelle?
Ans. It is triangular in shape.
Q45. Name the other fontanelle present & where is it situated?
Ans. It is sagittal fontanelle. It is inconsistent in its presence. When present, it is situated on the sagittal sture at the junction of anterior 2/3rd and posterior. It has no clinical importance.
Q.46. Define sub-occipito Bregmatic Diameter?
Ans. It extends from the nape of the neck to the centre of bregma. it is 9.5cm.
Q.47. Define Sub-occipito frontal diameter?
Ans. It extends from the nape of the neck to the anterior end of the anterior fontanella or centre of the sinciput. It is 10cm.
Q.48. From where does oocipito frontal diameter extend?
Ans. It extends from the occipital eminence to the root of the nose [Glabella]. It is 11.5cm.
Q.49. From where does mento-vertical diameter extend?
Ans. It extends from the mid-point of the chin to the highest point on the saggital suture. It is 14cm.
Q.50. Define Sub-mento-vertical diameter?
Ans. It extend from the junction of floor of the mouth and neck to the highest point on the suggital suture. It is 11.5cm.
Q.51. Define the sub-mento bregmatic diameter.
Ans.It extends from the junction of floor of the mouth and neck to the centre of Bregma.
Q.52. List the Transverse diameter concerned with mechanism of labour.
Ans. These are:
(a) Bi-Parietal diameter. (9.5cm)
(b) Super-sub Parietal diameter. (8.5cm)
(c) Bi-Temporal diameter. (8cm)
(d) Bi-Mastoid diameter. (7.5cm)
Q.53. From where do the bi-parietal diameter extend?
Ans. It extends between 2 parietal eminences. It is 9.5cm.
Q.54. From where do the sub parietal diameter extend?
Ans. It extends from a point placed below one parietal eminence to a point placed above the other parietal eminence of the opposite side.
Q.55. From where does the Bi-temporal diameter extend?
Ans. It is the distance between the anterior-inferior ends of the coronal suture.
Related Queries:
human development in the womb | abdomen physical exam | stomach examination | ultrasound fast exam | abdominal exam | us abdomen and renal tract examination | abdominal examination | abdominal assessment