ABDOMINAL EXERCISES | PELVIC EXERCISES
RESISTED KNEE TO CHEST
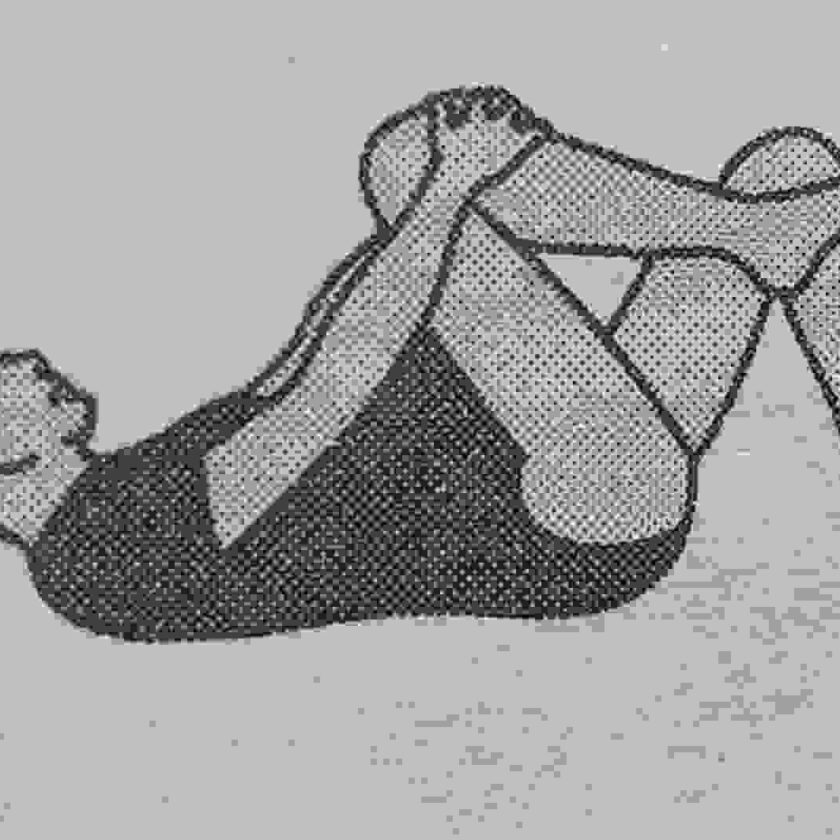
lie flat on your back with your knees bent and your feet flat on the floor start with a pelvic tilt and then lift your head toward your chest as you raise one knee towards your abdomen. Grap your leg just below the knee using both hands. Using your leg muscles, try to push the knee towards your feet while your hands pull the knee toward your feet while your hands pull the knee towards your abdomen. Hold for a count of 5, then relase. Repeat on the opposite knee. Do this exercises 5 times at first. Build up to 10 repetitions.
Pic: Mother performing resisted knee to chest exercises.
STRAIGHT CURL-UP
Lie flat on your back with your knees bent and feet flat on the floor. Bring your chin to your chest as you exhale, continuing forward for about 8″ (20 cm).
Pic: Mother performing straight curl-up exercises.
Be sure to curl your back without raising your waist. Then roll back down. Repeat this curl up 5 times at first. Build up to 10 repetitions.
PELVIC EXERCISES
Pelvic tilt on all fours

Position yourself on your hands and knees with your head and back paralled to the floor. Tighten your stomach muscles and tuck your buttocks under to round the lower back. Hold for a slow count of 5, then release. Do not hold your breath. Repeat this pelvic tilt 5 times at first. Build up to 10 repetitions.
Pic: Mothers performing pelvic tilt on all fours.
Pelvic floor or kegel Exercises
Tighten your pelvic floor muscles by squeezing the urethral and vaginal openings (you can identify those muscles by trying to stop your urine flow). You should feel the pevlic floor rise hold for a count of 5 and release. Repeat 5 times for a set, and perform a set 8 to 10 times each day.
Lower back and thigh muscle exercises
Lower back exercises can relieve lower back strain and promote good posture. They also will improve abdominal muscle tone, whichs helps support your growing uterus, deliver your baby, and protect your lower back during pregnancy and throughout life.
Pelvic floor muscles support your pelvic organs (the intestines, bladder and uterus) and help control then waging and anus. During pregnancy, exercisse of pelvic floor muscles can increase their strength, giving your greater control and ability to relax during delivery. They can improve healing, strength and bladder control after childbirth.
Tailor (Indian Style or cross legged) sit and stretch
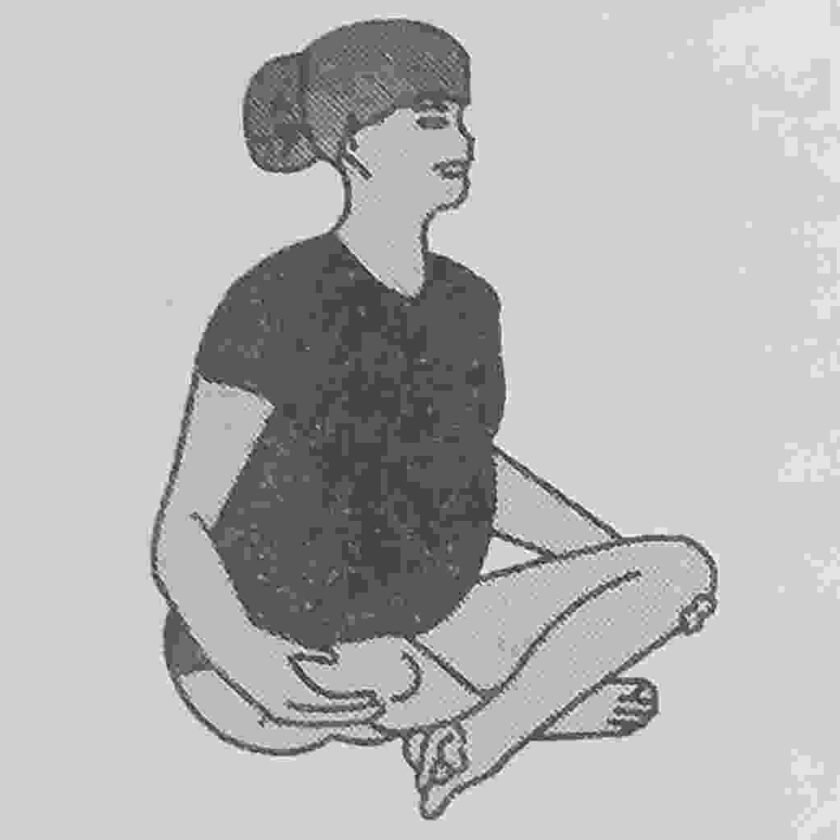
Sit on the floor with your knees out and ankles crossed. Hold your back erect to avoid slouching. While in this position, place your hands under your knees. Then press your knees towards the floor while resisting this movement with y9our hands. Hold for a count of 5, then release Do this stretch 5 times at first. Build up to 10 repetitions.
Pic: Mothers performing Tailor (Indian Style or cross legged) sit and stretch
ASSESSMENT CHECKLIST DURING EACH STAGE OF PREGNANCY AND DELIVERY
To be sure that you are assessing your patient thoroughly, use this handy checklist during each stage of pregnancy and delivery.
(a) Antepartum Period
(i) Nutrient intake including unusual cravings
(ii) Morning sickness.
(iii) Learning needs related to pregnancy and prepration for labour and delivery.
(iv) Fetal activity.
(v) Uterine contracitons.
(vi) Support to mother.
(b) Intrapartum Period
(i) Woman’s fetus’s physiologic adaptation to labour.
(ii) Abnormal and unexpected findings during labour.
(iii) Woman’s and family’s psychological response to labour.
(c) Postpartal period
(i) Maternal bleeding
(ii) Uterine involotion.
(iii) Breast changes.
(iv) Neonates adjustment to the extra uterine environment including skin clour, respiratory effect, cardiac funtion and other physiologic parameters.
(v) Neonate’s feeding and elimination pattern.
(vi) Mother baby interaction.
(vii) Breast feeding.
(viii) Temperature maintainace.
(ix) Parents learing needs.
WARNING SIGNS OF PREGNANCY
(a) Bleeding/leakage per vagina
(b) Loss of excessive fetal movements.
(c) Severe and continuous headache.
(d) Blurring of vision.
(e) Flashes of light before the eyes.
(f) Epigastric pain.
(g) Persistent vomiting.
(h) Chills ans fever
(i) Dysuria
(j) Edema of face and abdomen.
INDICATIONS OF FETAL GESTATIONS AGE OF THE FETUS
(a) Uterine size compatable with gestational age of the fetus.
(b) Normal and regular fetasl movements.
(c) Fetal heart rise in range of 110-160/min
(d) Desired increase in maternal weight.
DETERMINING EXPETED DATE OF DELIVERY (EDD)
The EDD is calcuated by adding 9 calendar months and 7 days of the first day of the 100 womans last menstrual period e.g.
If L.M.P is 4/3/2005 then E.D.D would be 4/3/2005 + 9 months + 7 days=11/12/2005
FORCES OF LABOUR (4.P’S)
Passage – The pelvis.
Passage – The fetus.
Power – Uterine contractions.
Psyche- Maternal state of mind
TIMING OF EPISIOTOMY INCISION
The episiotomy should neither be too soon nor Too late e.g. in
Vetex: It should be given when the head in visible about 4-5 cm at vulva or just prior to crowning when the pernieum is well stretched and thinned.
Breech: Incsion is given if post-battocks are distending the perineum.
CONSEQUENCES OF EPISIOTOMY IF GIVEN TOO SOON OR TOO LATE
It made too soon
1. Breech – Profuse bleeding
2. Vertex – The levator ani muscles may get damaged.
If made too late
1.Supports of the neck of the bladder are weakened.
2.Pelvic floor is over stretched.
3.Brusised tissue do not heal well.
4 Mother and fetus is subjected to unnecessary stress and strain.
5.The purpose of episiotomy and defeated.
DIFFERENCE BETWEEN CAPUT SUCCEDENEUM AND CEPHALO HAEMATOMA
CAPUT SUCCEDENEUM
A) It is present at birth
B It may cross a suture
C) Tends to grow less
D) Disappears within 36 hours.
E) Is diffuse pits on pressure.
F) A double caput is always unilateral.
CEPHALO HAEMATOMA
1. It appears after 24 hours.
2. It never crosses a suture.
3. Tends to grow large.
4. Persists for weeks.
5. It is circumscribed and does not pit.
6. A double Cephalo haematoma may be bilateral.
EPIDOSIN (VALETHAMATE BROMIDE NF)
Action
It causes relaxation of spasm of smooth musice without causing any serious reaction.
It has got anti-cholinergic properties of atropine-
It acts on cervical musculature by dilating it smoothy.
INDICATIONS OF EPIDOSIN
All types of spasm of smothh muscles. Delayed dilatation of cervix.
POST NATAL EXERCISES | POST NATAL WORKOUT
AIMS
1. To strengthen muscles particularly those stretched during labour or pregnancy i.e. abdominals and Pelvic floor muscles.
2. To reduce excessive fat.
3. To maintain firm shape of breasts and secure their adequate milk supply.
4. To prevent painful feet on getting up.
5. To correct posture.
6. To restore mother’s morale and foster a confident attitude of mind.
7. To combat venous stasis.
ESSENTIAL POINTS ON PERFORMANCEOF EXERCISES
1. Before starting and after finishing exercises-must practice deep breathing.
2. Never hold breath whilst performing and exercise.
3. Relax all muscles at the finish of each exercise.
4. Exercises must be done in a controlled and rhythmical manner.
5. If patient feels tired after exercises practice them less sternously.
6. Patients with haemorroids, may find some discomfort with exercises. She should perform only with the exercies which she is able to do easily.
POST PARTUM EXERCISES
Should start 24 hours after delivery. Do all exercises five times a day.
Ist Day
1. Face lying with pillow under abdomen for
30 minutes empty stomach. Breathing exercises-Back lying. 2.
(i) Hands placed on sides of chest, breathe in to expand chest sideways and out.
(ii) Hands in abdomen. Breathe in a tummy out and breathe out and tummy in. 3. Back lying. Move feet up and down and in and
out. Back lying. Press in both legs and relax. 4.
IInd Day
1. Face lying lifting head and neck.
2. Back lying with legs crossed at ankle..
(i) Press the thigh from the back.
(ii) Press the buttocks in and relax. (iii) While doing the above two exercise pull the urethera, gagina and anus as though to prevent micturation and dacfication.
3. Back lying with hops and knees bent.
(1) Press in both knees and relax. (ii) Bend alternate knee towards chest.
4. Arm circling exercises for breast. Hands on shoulders, move elbows upwards, sidewards, backwards and downwards.
IIIrd Day
Position back lying with hops and knees bent. 1. Keeping knees pressed in, lifting the pelvis. 2. draw in the lower abdominal wall so that whle of lower back lies in contact with the bed, later buttocks off the bed by putting weight on heels. Relax and then tighten the back muscles so that both fists can be pushed between the hollow of the back and the bed.
3. Same position with hands above the shoulder level. Bend both knees towards.
IVth Day
Position back lying with hops and knees bedn.
1. Keeping knees pressed in, lifting the pelvis.
2. Draw in the lower abdominal wall so that whole of lower back lies in contact with the bed, later buttocks off the bed by putting weight on heels. Relax and then tighten the back muscles so that both fists can be pushed between the hollow of the back and the bed.
3. Same position with hands above the shoulder level. Bend both knees towards one side any try to touch them with the bed. Relax and repeat on the other side..
4. Breast exercises: Raise the arms to shoulders. Level and cross them infront so that right hand clasps under (L) elbow and left hand under (R) elbow. Breathe in and with a souccession of quick jerks. Grip your forearm and try to push the skin towards elbows. Jerking movements tighten the breast muscles.
Vth Day
1. 2. Face lying lifting head and shoulders..
Back lying with hops and knees bent. Hands up is air, lifting head and shoulder off the bed i.e. trying to sit up.
3. Back lying with arms by the side of the body, lift your head off teh pillow stretching the left hand on to the right thigh. Keeping the right shoulder on the bed.
4. Back lying, lift one leg straight up and then other and then both together.
VIth Day
1. Face lying, lift the shoulder and back. 2. Back lying. Bend up both knees and at the same time lift up had and shoulders and try to touch nose with the knees.
3. Postural correction exercises: Stand with your feet apart and 3 away from a straight wall. Breathe in and slowly unroll your spine, pushing first the hips, then the small of back against wall. The relax:
INSTRUMENTS USED IN OBSTETRICS | Gynecological Instruments
Common instruments used for various gynaeocological and obstetrical operations
Instruments and Use:
1. Sims Vaginal Speculum: To inspect the posterior = vaginal wall during P/V examinations.
2. Vaginal Speculum (Cusco’s): To inspect the cervix and the vaginal vault.
3. Fergusson’s Vaginal Speculum: To inspect the cervix, to hold cervical wall for the application of some medicine in the cervix and vaginal vault.
4. Auvardz: This is a self retaining vaginal speculum.
5. Vaginal Retractor: Used for elevating anterior vaginal wall.
6. Sponge Holding Forceps : Used for application of antiseptics, also used for removal of uterine polyp, for grasping wall of the cervix in gravid uterus.
7. Vulsellum: Multiple teeth with internal curve to grasp the cervical lip.
8. Vulsellum Single Toothed: Used for grasping small cervix.
9. Uterine Sound: Used for measuring the length of the uterine cervity and its position.
10. Uterine Cervical Dilator : Used for dilating cervical canal for various operations.
11. Uteine Curette: Scraping of the endometrium lining of the cavity of the uterus and cervical canal.
12. Blunt Flushing: Used for the removal of placental polyp chorio-carcinona.
13. Uterine Forceps: Used to dress the uterine cavity with sterik gauze 30 pieces and antiseptic. It is used as a laminant introducer.
14. Lane’s Tissue Forceps : It is used for removal of uterine polyp.
15. Alli’s Tissue Forceps: To use for vaginal plastic repair operations to holup peritoneal margins.
16. Hysterectomy Clamp Forceps: Clamping the ligament and peritoneal wall.
17. Angular Scisors Bend on Flat: Used for anterior colporrhaphy operation.
18. Bladder Retractor : Used for retracting urinary bladder inwards in Mayo’s operation. Also used as a vaginal retractor in vaginal tubal ligation. Right angle’s/Langerhan’s retrractors are available of different sizes.
19. Cat’s Paw Retractor: To use for eventration of the uterine fundus in ward-myos operation. 20. Martin’s trocer: Used for drainage of pelvic abscess.
21. Histerosalpingo Graphy Cannula with Syringe: Used to check the patency of fallopian tubules.
22. Doyen’s Abdominal retractor
23. Ovarian Cyst Holding Forceps: Used for removing the cyst from the ovary.
24. Ovarian Cyst Forceps : Used for compressing the opening in ovarian cyst while trocar is being withdrawn in the tubing the ovarian cyst.
25. Round ligament Forceps: Used for holding round ligaments.
26. Needle Holder: Used for holding needle for different operations.
27. Bonney’s Clamp: Used for controlling blood supply through uterine arteries and the cervix.
28. Willefts Scalp Forceps: Used in placenta praevias head delivery in lower segment ceassarian section foetal head the in proplapse.
29. Ovum Forceps: To remove the seperated product of the conception from the uterus.
30. Blunt flushing Curette : Curetting may be done in uterine evacuation by this.
31. Kocher’s Artery Forceps : Low rupture of membrane, clamping the umblical cord to deliver the membrane.
32. Green Armytage Uterine Forceps : Used for clamping the edge of the lower uterine segment in caessarian section operation for homeostasis as well as fraction.
33. Perforator Oldhams: Used to perforate the foetal head.
34. Cephalo Tribe: Used for crushing and extracting the perforation.
35. Babcorck: To hold fallopian tubes in tubectomy. 36. Mercom Sucker.
37. Sucker.
38. Endotracheal Tube : Newborn Adult
39. Rubber Catheters
40. Myomectomy Clamp.
41. Endometerial biopsy.
42. Myoma Serew Curettes.
NURSING DIAGNOSIS
1. ECTOPIC PREGNANCY
(a) Risk for fluid volume deficit R/T blood loss from ruptured tube.
(b) Pain R/T ectopic pregnancy or rupture and bleeding into the peritoneal cavity.
(c) Anticpatory grieving R/T loss of pregnancy and
potential loss of childbearing capacity.
2. HYDATIDIFORM MOLE
Potential for fluid volume deficit R/T maternal
heamorrhage. Anxiety R/T loss of pregnancy and medical intervention.
3. SPOTANEOUS ABORTION
Anxiety R/T loss of pregnancy cause of the
abortion future child bearing.
4. HYPEREMESIS GRAVIDARUM
(a) Risk for fluid volume deficit, electrolyte imbalance R/T prolonged vomiting.
(b) Altered nutrition less than body requirements R/T prolonged vomiting.
(c) Ineffective individual coping R/T stress of pregnancy and illness.
(d) Fear R/T concerns for fetal well being.
5. PLACENTA PRAEVIA
Altered tissue perfusion, placental, R/T excessive bleeding causing fetal compromise. (a) Fluid volume deficit R/T excessive blood loss and
open vessels near cervix.
6. ABRUPTIO PLACENTAE
(a) Altered placental tissue perfusion R/T excessive bleeding, hypotension and decreased cardiac output.
(b) Fluid volume deficit R/T excessive bleeding. (c) Fetal compromise R/T excessive bleeding, procedures and unknown outcome.
7. HYPERTENSIVE STATES OF PREGNANCY
(a) Fluid volume excess R/T pathophysiologic changes of PIH and increased risk of fluid overload.
(b) Altered tissue perfusion, fetal cardiac and carebral R/T altered placenatal blood flow cause by vasospasm and thrombosis.
(c) Risk for injury R/T convulsions.
(d) Anxiety/Knowledge defict R/T diagnosis and concern for self and fetus.
(e) Diversional activity deficit R/T prolonged be rest.
(f) Decreased cardiac output R/T decreased preload or anti-hypertensive therapy.
8. Pohyhydiamnios :
(a) Ineffective breathing pattern R/T pressure on diaphragus.
(b) Altered tissue perfusion, placental R/T pressure from excess fluid.
(c) Impaired physical mobility R/T edema and discomfort from the enlarged uterus.
(d) Anxiety R/T fetal outcome.
(e) Risk for injury R/T over distension of the ut and possible heamorrhage.
Complications of Labour
9. Preterm loabour :
(a) Anxiety R/T medication and fear or outcome pregnancy.
(b) Diversional Activity deficit R/T. prolonged rest.
(c) Risk for injury to fetus, secondary to B sympathomimetic tocolytics.
(d) Risk to fetus secondary to prematurity. (e) Ineffective family coping: Compromise secondary hospitalization.
10. Induction of Labour:
(a) Anxiety related to planned childbirth outcome.
(b) Altered tissue perfusion, uteroplacental with altered oxygen to fetus related to strength uterine contractions.
(c) Pain related to uterine activity.
11. Rupture of uterus
(a) Fluid volume deficit related to active fluid low from Haemorrhage.
(b) Altered tissue perfusion, maternal vital organ and fetal related to hypovolemia.
(c) Fear related to surgical outcome for fetus and mother.
12. Episiotomy:
(a) Risk for infection R/T traumatized tissue.
(b) Pain R/T surgical procedure;
13. Forceps Delivery
(a) Anxiety R/T fetal outcome.
(b) Pain R/T procedures.
14. Casaerean section
(a) Anxiety R/T surgical procedure.
(b) Pain R/T surgical procedure.
(c) Risk for infection rito traumatized tissue.
(d) Risk for ineffective parent/infant attachment R/T interruption in bonding process.
15. PPH
(a) Anxiety R/T unexpected blood loss and uncertainity of outcome.
(b) Fluid volume deficity R/T blood loss.
(c) Risk for infection R/T blood loss and vaginal examination.
16. First stage of Labour:
(a) Altered nutrition less than body requirement related to food restriction during labour.
(b) Fluid volume deficit R/T decreased oral intake.
(c) Anxiety R/T concern for self and the fetus.
(d) Pain R/T uterine contraction and for position of the fetus.
| ReplyForward |